Since January, Dr Arifa Parker has served at the coalface of South Africa’s fight against Covid-19. Biénne Huisman chats to her about what life is like in the eye of the storm.
When she gets home in the afternoon, physician Dr Arifa Parker disposes of her work clothes in the washing machine. She then has a thorough shower before greeting her three-year-old twin toddlers, Yusra and Haniya, with a hug.
Since January, Parker has served at the coalface of South Africa’s fight against the Covid-19 coronavirus. As one of three infectious diseases specialists at Cape Town’s Tygerberg Hospital, she treats patients positive for the virus in specially set up wards.
Meanwhile, she is also gathering information and formulating protocols for how to best tackle this pandemic.
This week, 39-year-old Parker opened up to Spotlight about being a doctor and a mother in the eye of the Covid-19 storm. Speaking via a Zoom interview, her sentences are laced with laughter, despite the gravity of the task ahead of her.
“I’m very careful,” she says.
“I know what the risks are and when I see my patients, I make sure that I wear adequate PPE [personal protective equipment]. And that is what I tell the junior staff as well. No one should be seeing patients without adequate protection. We do have enough stock for now – if we use it wisely – and more has been ordered,” Parker says.
“So that makes me feel better going home to my kids. I jump into the shower and wash my clothes before giving my little ones a hug. That is a bit odd because they usually would jump into my arms immediately when I get home.”
Fortunately, Parker’s husband, Ghaliel, who works in information technology, is taking care of their young children during lockdown.
“He’s been amazingly supportive,” she says.
“He’s been working from home via Zoom, with the kids in the background.”
HIV and TB
Parker’s early training is in HIV and tuberculosis (TB). After completing a medicine degree at Stellenbosch University, she did her internship at GF Jooste Hospital in Manenberg, on the Cape
Flats, under renowned mentor Professor Graeme Meintjes. This was in 2005, a year after antiretroviral (ARV) drugs were first rolled out by the state in South Africa.
“At the time it was quite overwhelming because ARVs were not freely available and a lot of young people were dying,” recalls Parker.
“You know, as interns we used to have to fill in the death certificates. So you would have the deceased in front of you and you’d look at the ID photo and it would show someone so different to the completely ravaged patient. That’s why I ended up doing internal medicine and infectious diseases, because I wanted to understand a bit more about how the body works and how one could be able to treat these patients better.
“You know, it’s actually quite rewarding to work in the field of HIV medicine. But we still have a lot of work to do. We still have lots of challenges – TB and everything else.”
She pauses as her phone rings. She excuses herself to answer it, then turning back to the interview she adds: “And now there’s Covid-19 thrown into the mix too.”
On January 11, Chinese state media reported the first known Covid-19-related death. Since then, Parker has “lived and breathed” Covid-19.
“Covid didn’t exist to us before January,” she says.
“We heard about it mid-January and then we started having to prepare for cases, having to put procedures and systems in place. So as infectious diseases specialists, we’ve had to educate ourselves rapidly. We’ve had a steep learning curve and part of that has been adapting to create standard operating procedures for our hospital.”
Days blur and merge
“Since January, my days have all blurred into one,” she says.
“Most days I can’t remember what day it is. I haven’t been sleeping much since the start of Covid, I mean, this morning I woke up at 4:30am. As you know, Covid-19 is a new infection with new data coming out all the time, so the first thing I do is look at my phone. I get lots of messages, so I read the new things and send it on. My work day at the hospital starts at 8am; at 9am we have what we call a Covid ops meeting, where all our hospital’s heads meet – radiology, surgery, anaesthetics, intensive care unit and so on.”
She gets home at around 5pm – sometimes.
“For example,” she says, “last Friday at 4pm, 200 people suddenly rocked up at the hospital’s testing centre at one time. I mean, you can’t just leave junior staff alone, so a few of us senior staff stayed behind and helped out and assisted in doing the tests.”
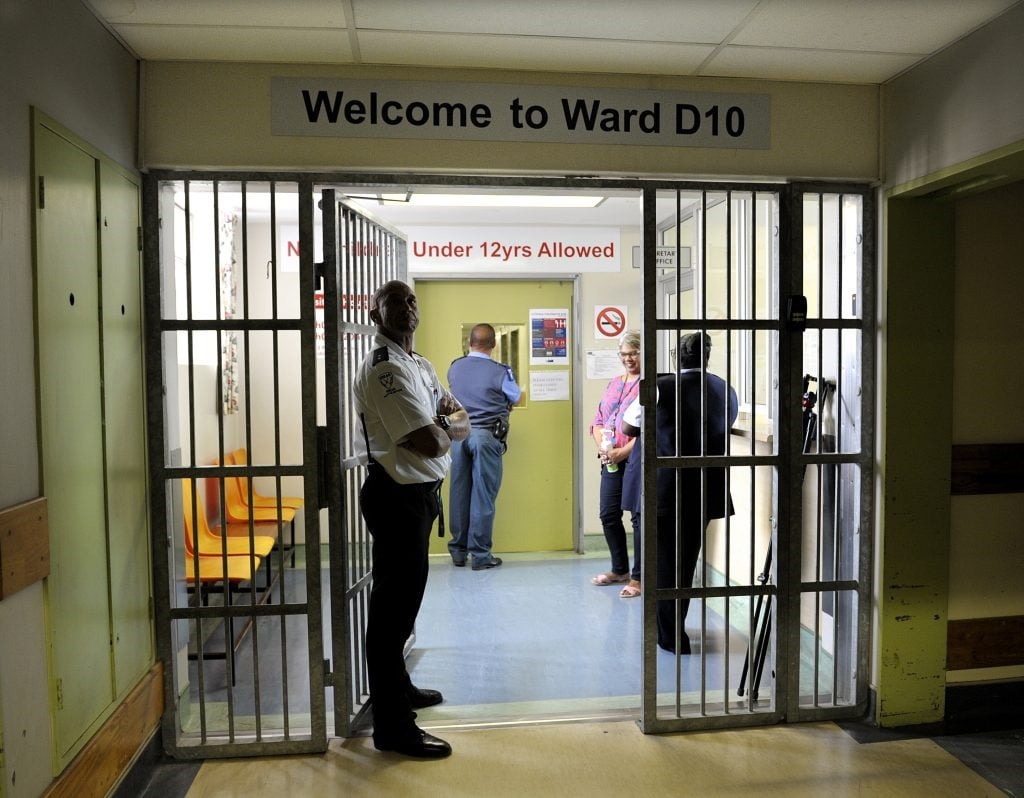
While Parker cannot comment on patient figures, she says at present Tygerberg has two general wards full and is ready to activate more. She is quick to deflect praise, crediting her team and colleagues.
“It’s been a hospital response from all departments. I feel so privileged to be working with such amazing people at my hospital,” she says.
Changing demographics
Parker points out that the demographics of the Covid-19 outbreak are changing. Initially, transmission was travel-related. Now healthcare specialists are seeing the early stages of community transmission. Of great concern is increasing transmission to essential workers.
She notes a spike in infections in Khayelitsha. According to provincial statistics released by Western Cape Premier Alan Winde on April 28, there were then 205 confirmed Covid-19-positive people in the township.
“Last week, my direct boss, Neshaad Schrueder, and I went to Khayelitsha Hospital,” she says.
“We were concerned about the spike in Covid-19 numbers and wanted to see how Tygerberg could support the hospital. I think they have an excellent team of staff. They’ve put amazing systems in place; they’ve also started a tent for testing outside the hospital and within the hospital they’ve identified separate spaces where they can keep persons isolated from each other. So we were able to help with that,” she says.
“We’re also advising hospitals that we need to work together, so if they are seeing that they are overrun with patients they shouldn’t hesitate to call us because it’s pointless having open beds in one hospital while another is full. We know [that] Covid-19 sort of attacks areas, so you’ll have fires of outbreaks and one area might have more cases, especially at this point in the outbreak.”
Time to prepare
Can the pandemic still be contained in South Africa? “Obviously we’re worried,” says Parker.
“I don’t think we can entirely eradicate Covid-19. I think it will be a problem, but I think it’s imperative that we try to prevent cases. We are obviously concerned about overcrowded areas and that is why the country has rolled out community testing.”
While government is under fire from some quarters for its lockdown regulations, Parker insists these measures are crucial.
“My personal opinion is that the lockdown was an excellent decision because it gave our hospital and other hospitals time to prepare; time to make sure that staff is educated on how to use PPE; time to create ward and intensive care space; time to create the documents that we are working on at the moment,” Parker says.
She says healthcare workers are rethinking the way in which they practice medicine in the time of Covid-19.
“We have to minimise risk while assessing and managing patients,” she says.
“As physicians, we love to spend time with patients. We love to feel, touch and to thoroughly examine everything. But I think we need to sort of rethink the way we practice medicine in the time of Covid-19; having an additional layer of awareness.”
How do they compensate for a lack in physical interaction?
“Our patients have been amazing,” says Parker. “I’ve also learned new things about technology – communicating via cellphone, phoning the patients and taking their history like that, asking them if they are okay. I have renewed respect for social media [because it] is really helping to keep patients in touch with their families.
“Somebody mentioned that maybe we should have patients not have their phones with them because they can get contaminated. That’s the worst idea. This is the way they keep in touch with family and friends, despite the lack of interaction.”
Parker adds that the public and private health sectors are collaborating in the fight.
“This has been another amazing thing. We call each other for advice; it’s just been such a different experience as to how medicine normally works. I really hope that we continue this sort of enthusiasm [post-Covid-19].”
This article was produced by Spotlight, an online publication monitoring South Africa’s response to TB and HIV




 Publications
Publications
 Partners
Partners